The track at Amherst Regional High School is like a second home to me. I graduated from Amherst Regional in 1983 and have been teaching history there for the past 21 years. I also coach the cross-country and track teams. The place is one of my primary comfort zones.
I particularly enjoy the track on summer mornings when I don’t have to report to classes afterward. Last July 26, a Tuesday morning I’ll long remember, I began my interval workout early, at 6 a.m. I wanted to sharpen my speed for the New England Grand Prix road race championships, which I generally enter. I've run a 1:13:01 half marathon and averaged 25 miles a day during a trans America run in 1991, so I’ve been at this for awhile.
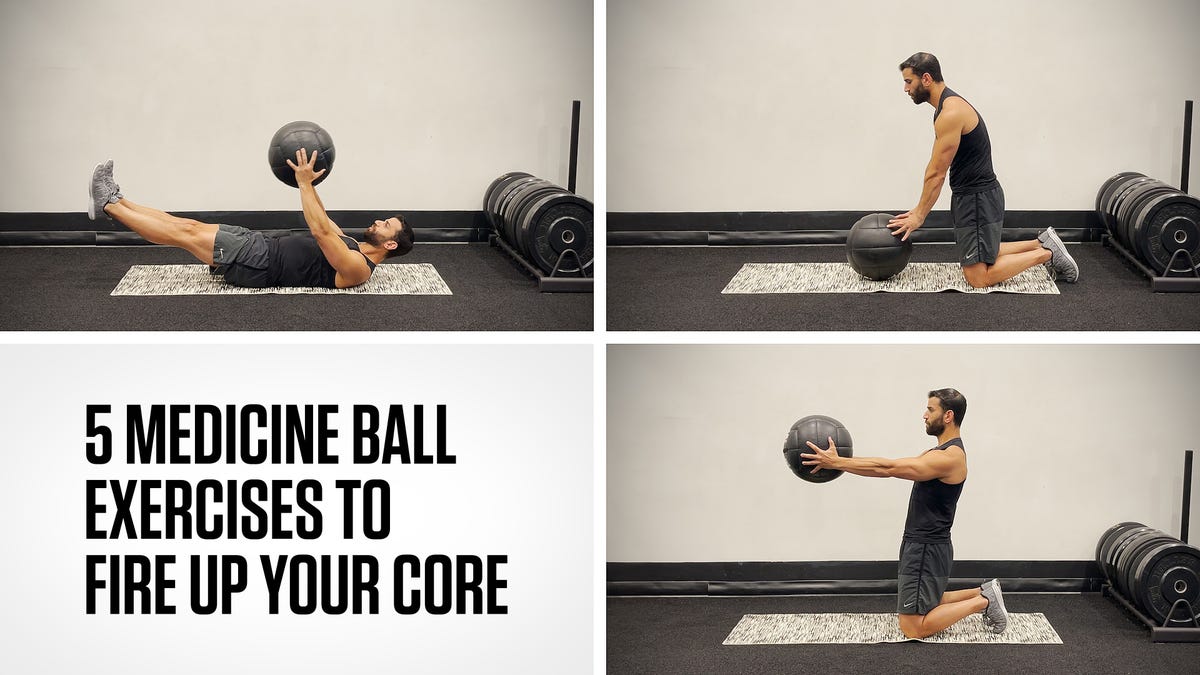
I began my track workout with a 5:32 for 1600 meters—83 seconds per 400. Good effort for a 50-year-old. Next I stepped down the ladder to 1200 meters, planning to run 81 seconds per lap. The first was fine, 80. The second disappointing, 83. And the third? I don’t know what to say. The bottom fell out. I ran an 89.
When I sat down to rest and think about things, I noticed that my arms and chest were sore. They felt as if I had done an unusually heavy strength-training workout the day before. Only I hadn’t.
At the time I was mostly discouraged by the dismal 89-second lap. I didn’t know then that it could have been my last lap ever.
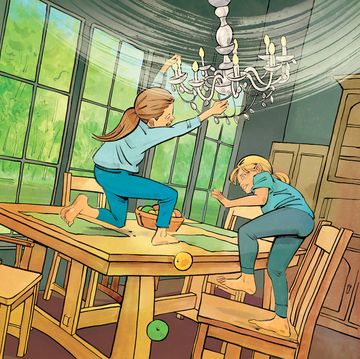
I drove home, rested briefly, and wondered why my upper body continued to feel vaguely uncomfortable. My wife, Debbie, also a serious runner, thought I was acting strange. “Are you alright?” she asked. “You don’t seem youself. Maybe you should go to the doctor.”
I felt almost insulted. “Why would I do that?” I asked her. “There’s nothing wrong with me. I just need a little recovery.”
A few minutes later, I showered, dressed, and took my daughter to summer school. Then I stopped off at the bank to deliver a church deposit. That should have ended my morning rounds.
But I kept hearing Debbie’s voice in the back of my head. Almost before I knew it, I found myself driving to the UMass Health Center in Amherst to get checked out. I’m generally quick to visit a doctor. Sometimes I wonder if I have too much faith in medical professionals. When I have a minor running injury, for example, I get it looked at pretty fast. I don’t sit around and wait three months like a lot of runners. And my cancer doctors really came through for me in 2003 when I survived late-stage testicular cancer.
Still, I figured the physicians would dismiss me in about five or 10 minutes. They took my blood pressure—only slightly elevated. And gave me an EKG test—it looked fine. Nonetheless, they told me that my physical descriptions amounted to a red flag. They wanted to put me in an ambulance and transfer me to Cooley Dickinson Hospital in Northampton. Well, okay. I guess. But why? (Thanks for insisting, Doc.)
At Cooley, a blood test revealed an elevated level of cardiac troponin, an enzyme released when the heart muscle is injured by a heart attack. That evening, I was transferred again, this time to Baystate Medical Center in Springfield. The next morning, a surgical team inserted a stent into one of my cardiac arteries, where a cholesterol clot had caused the heart attack. Three days later, I was released.
For the next four weeks, I was told not to run. Just to walk. I generally did three to four miles a day at anywhere from 16 minutes to 13 minutes per mile. Next came four weeks of cardiac rehab on treadmills while supervised by doctors. I walked, then began running.
It felt easy, but the doctors had a precise protocol they wanted me to follow. I was only too willing to go along with it. None of us wanted to rush things. We wanted to inch forward step-by-step while my heart function was being monitored.
Eventually I got to the point where I covered four miles at 6:20 pace in the rehab lab. After that, they let me go, warning only that I shouldn’t race all-out until 12 weeks had passed since the surgery. In September, I returned to teaching and coaching, something that has always meant a lot to me. I love spending time and effort outside with young runners. We learn plenty from each other, and our cross-country teams have been very strong. We won the state title in 2001 and have been in the top 10 many times in last 20 years.
Debbie and the members of our Shutesbury Coffee Cake Running Club played a big role in my running recovery. They were so supportive. I never had any real fear about my comeback, because my cardiology team was so convinced I could return to my normal running. But you need every bit of help and encouragement you can get.
By early December, I was ready to join my teammates on the Greater Springfield Harriers at the USATF National Club Cross-Country Championships in Tallahassee, Florida. I knew I probably wouldn’t score on our strong 50+ team, but I wanted to race with my friends again at the national level. As it turned out, I placed seventh on our team that day—running the 10K cross-country course in 37:40—and we won the team title.
More than anything, it felt great to be on a starting line again. I might be getting older and slower, but I still love the feeling I get from serious competition. It was a rewarding day all-around.
As I write these words in mid-February, I’m training anywhere from 35 to 50 miles a week and feeling as good as ever. I’m on several heart medications and paying a little more attention to my diet. My total cholesterol level was high, 241, at the time of the heart attack, and I am eating less meat and dessert now, but my weight hasn’t changed. (I’m 5-foot-9 and 150 pounds.) I look forward to many more years and many more races.
I often think back to the July morning when this story began. The first thing that comes to mind is that it was nothing compared to cancer. My cancer battle lasted a year, and involved surgery, chemo, and more surgery. That morning last July my pain level never moved beyond 2 on a 1-to-10 scale. I just thought I was having a rough day on the track.
I can’t help but marvel how the simple math on my watch set everything in motion. A runner like me shouldn’t just go from an 83-second lap to an 89. Something was wrong!
Whenever I recounted this anecdote to my cardiologists, they were fascinated that an athlete could gauge things so precisely and recognize when something was out of whack. They almost never see that degree of exercise sensitivity in their other patients. It made me glad to be the type of runner who knows himself, has a plan, and times his workouts.
I am incredulous about other family heart events that occurred at the same time as mine. An uncle died of heart failure two weeks before my episode, and a perfectly healthy mother-in-law needed to have a pacemaker implanted. She and I were released from our hospital on the same day.
I keep returning to another key moment. Debbie had a sense that I was not my usual self before I did. Sometimes your spouse or closest friends are the first to dial into your condition.
It’s a good idea to listen to them.