If you’ve ever had a urinary tract infection, you know the unique agony of a terrible burning feeling and relentless need to pee all wrapped up in one nightmare scenario.
Up to 60 percent of women will have a UTI at some point in their lifetime, and 1 in 4 will experience recurring infections, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). While men can get them, too, women are much more likely to contract one.
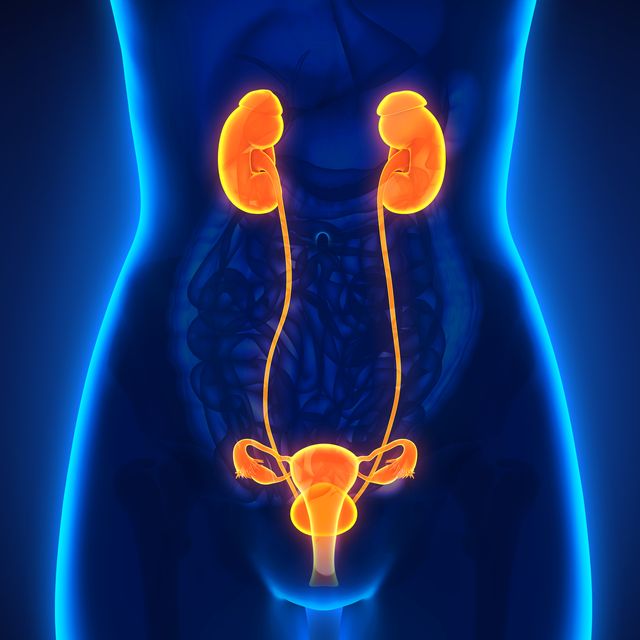
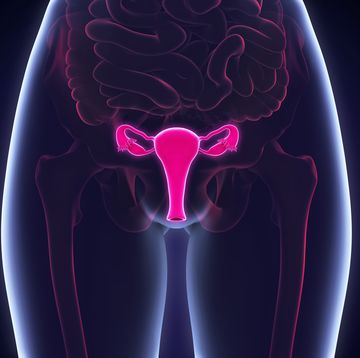
You can blame anatomy for this. (Thanks, anatomy!) Women have a shorter urethra (aka, the tube that urine flows out of) than men, which makes it all too easy for UTI-causing bacteria to pass through it and invade the bladder.
“Our urinary tract system is designed to keep out bacteria; however, these defenses can fail,” says Kelly M. Kasper, MD, an ob-gyn at Indiana University Health. “When that happens, bacteria can grow, multiply, and cause infections.” Common symptoms of a UTI include painful urination, a strong urge to urinate with little relief, discolored or strong-smelling urine, pelvic pressure or pain, extreme fatigue, and sometimes even a fever if the infection has become more serious.
It’s important to emphasize that a urinary tract infection is common, so you shouldn’t be too embarrassed to seek care when symptoms strike (a prescribed course of antibiotics will get rid of symptoms quickly). In fact, delaying treatment can lead to serious complications, like a kidney infection.
Of course, the best thing you can do is prevent UTIs from forming in the first place—but to do that, you need to know what causes them. Here, the most common UTI causes in women, plus tips on what you can do to prevent them.
Sex
Many women get UTIs after sexual intercourse because the motion can transfer bacteria from the bowel or vaginal cavity into the urethra. To lower your risk, pee within 30 minutes before and after being sexually active, says Lisa N. Hawes, MD, a spokesperson for the American Urological Association. Washing up after is never a bad thing, but avoid using lots of soap products. Research also shows that the use of diaphragms and spermicides can bump your chances of developing a UTI.
Menopause
UTIs are very common in women after menopause, Kavita Mishra, MD, a urogynecologist at Stanford University, recently told Prevention. That’s because your estrogen production to drops, resulting in vaginal pH changes. This disturbs the balance of bacteria and yeast in the vagina, increasing chances of infection. Some postmenopausal women with atrophy (aka thinning of the vaginal walls) can also develop small cuts near the urethra, which may predispose them to UTIs.
Constipation
Your poop (or lack thereof) is a UTI cause to be aware of. Being constipated makes it difficult to empty your bladder completely, which means trapped bacteria have lots of time to grow and cause infection, says Dr. Hawes. On the flip side, diarrhea or fecal incontinence can also increase your risk of getting a UTI, because bacteria from loose stool can easily make their way into your vagina and urethra. A tried-and-true tip: Wipe from front to back after you go to the bathroom to prevent bacteria transfer.
Uncontrolled diabetes
“When blood sugar is high, the excess sugar is removed through the urine,” Dr. Hawes says. “This makes a favorable environment for bacterial overgrowth,” potentially leading to infection. What’s more, people with diabetes have a weaker immune system, which makes it difficult to fight off infection-causing bacteria. You may have heard that eating too much sugar causes UTIs, but Dr. Hawes confirms that unless you have diabetes, your sweet tooth isn’t the culprit.
Holding in your urine
If you have to go, go! “Holding our urine for 6 hours or more may make UTIs more common, as bacteria that does get into the bladder has lots of time to overgrow between voids,” Dr. Hawes says. While traveling, for example, it may seem like a good idea to hold tight and keep driving until the next rest area, but do yourself a favor and stop—the extra miles aren’t worth the risk of a UTI.
Dehydration
Drinking plenty of water not only quenches your thirst, but it also wards off UTIs, according to the NIDDK. When you pee regularly, your body is able to flush out any bacteria that could fester in your urinary tract, so aim to drink six to eight 8-ounce glasses of water daily to help prevent an infection, the NIDDK says.
Feminine products
“Dirty pads and tampons are a place where bacteria can grow very easily,” says Ehsan Ali, MD, a primary care physician in Beverly Hills, California. To prevent urinary tract infections during your menstrual cycle, change your tampon at least every 4 hours, depending on your flow, and avoid wearing them overnight. Pads should also be changed every 4 to 6 hours.
Uncomfortable underwear
Your underwear may also be a surprising UTI cause, according to Alyssa Dweck, MD, a practicing gynecologist in New York. She says wearing breathable, cotton underwear helps prevent excessive moisture that causes bacteria to grow down there. “Avoid thongs with a thin, chafing G-string, which can transfer bacteria,” she says.
Kidney stones
Kidney stones are hard mineral deposits that form inside of your kidneys. Because they can block the urinary tract and back up urine, kidney stones can cause urinary tract infections by giving bacteria plenty of time to grow, says Dr. Ali. In turn, delaying treatment for your UTI can lead to potential kidney damage, so be sure to seek care ASAP if you feel any common UTI symptoms.
Stay updated on the latest science-backed health, fitness, and nutrition news by signing up for the Prevention.com newsletter here. For added fun, follow us on Instagram.
Angela Chaudhari, M.D., is an associate professor in the Department of Obstetrics and Gynecology at Northwestern University Feinberg School of Medicine. She received her M.D. from Northeastern Ohio Universities, completed her obstetrics and gynecology training at Washington University in St. Louis in 2004, and then completed a fellowship in mi
nimally invasive gynecologic surgery at Florida Hospital, Celebration. She serves as the chief of gynecology and gynecologic surgery at Northwestern Medicine, overseeing surgical quality and patient safety. She is also the founder and director of the P2P Network, a physician peer support program, that provides emotional first aid for physicians experiencing professional burnout at Northwestern Medicine. She is an executive leadership coach certified through Northwestern’s School of Education and Social Policy, Organizational and Leadership Coaching Certificate Program.
Clinically, Dr. Chaudhari focuses on providing individualized, equitable care for patients needing minimally invasive gynecologic surgical approaches for gender affirmation, abnormal uterine bleeding, uterine fibroids, and endometriosis. Her research interests are in surgical education, simulation and coaching, physician well-being and burnout, and leadership coaching for physicians and healthcare leaders.